How does diabetes affect eyesight?
At some point following diagnosis, many people with diabetes experience changes to their vision. Diabetes (type 1 and 2) can affect the blood supply to the eyes, which may contribute to the development of cataracts, glaucoma and diabetic retinopathy. So, for those with diabetes, it’s particularly important to have regular eye examinations to monitor eye health and detect any issues early.
What is diabetic retinopathy?
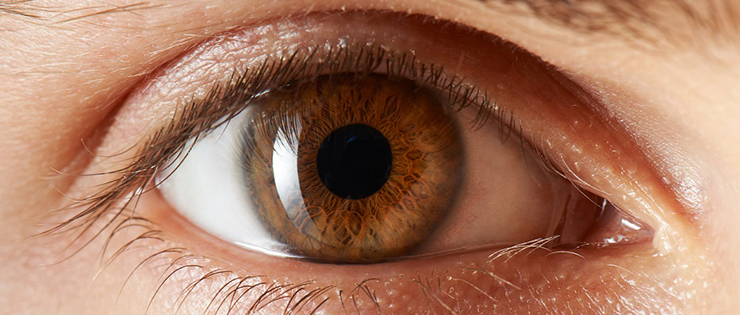
High blood sugar levels can damage the fine blood vessels of the retina, the light-sensitive lining at the back of the eye. This can result in blockage, blood leakage, swelling and inflammation, all of which can affect the vision. The condition is called diabetic retinopathy and it happens in two stages:
• Non-Proliferative or Background Retinopathy – This is the early stage when vision is not permanently lost but detection is important, to help prevent things getting worse. At this stage the vision may become hazy and straight lines appear bent.
• Proliferative Retinopathy - This stage is more serious and needs to be treated as soon as possible to prevent serious vision loss. Higher than normal blood glucose levels lead to the growth of new, very fragile blood vessels in the retina. They are more prone to bleeding which can cloud the vision, cause scarring and even lead to retinal detachment.
What are the symptoms?
Symptoms vary from person to person, but they include:
• Blurred vision.
• Floaters and spots.
• Blank or missing areas in the vision.
• Double vision.
• Difficulty seeing well at night.
• Problems with balance, reading, watching television and recognising people.
• Being overly sensitive to glare.
If you have any of these symptoms, regardless of whether you have diabetes, you should have an eye examination as soon as possible.
How is it diagnosed?
Diabetic Retinopathy is diagnosed when there is damage to the back of the eye is noticed in the form of small haemorrhages and leaky blood vessels. People with diabetes should have an eye examination at least once every 12 months, and more frequently if there are any early signs of diabetic retinopathy developing. Once your pupils have been dilated with eye drops to give a clearer view of the retina, your optometrist can perform a very thorough examination of the retina. Diabetics who are eligible Medicare card holders will generally be covered for this examination.
If you visit an OPSM optometrist they have access to ultra-wide digital retinal cameras which offer a 200-degree view of the retina, which is four times wider than a regular Digital Retinal Scan^. This technology can help detect diabetic retinopathy and record the appearance of the retina and monitor over time for any subsequent changes.
What is the treatment for diabetic retinopathy?
Good management of blood glucose levels may help delay the onset of diabetic retinopathy. But once it has been detected, your optometrist may refer you to an eye surgeon who will most likely carry out laser treatment. Lasers can be used to kill the newly grown blood vessels in the retina, causing them to clot. The treatment cannot restore lost sight, but it is most effective when diabetic retinopathy is in its very early stages, which is why early detection is so important.
If you have any questions or concerns, book an eye test at your OPSM store to take advantage of their eyecare technology and expertise visit www.opsm.com.au
^ Compared to a standard and more common 45 degree Digital Retinal
