
Bone marrow transplants are life saving operations for people who are very ill. The operations can only occur through the generosity of strangers willing to go through a procedure to give someone the gift of life. Here’s what you need to know if you’ve ever considered registering as a bone marrow donor.
What is Bone Marrow?
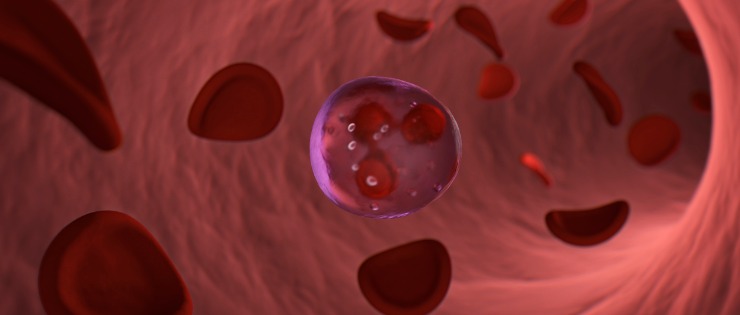
Bone marrow is the tissue found inside some of our flat bones such as the hips, ribs and skull. Our marrow contains stem cells which can turn into red blood cells that carry oxygen. Bone marrow also produces white cells needed to fight infection and platelets to stop bleeding. Red blood cells have a life of only three months so our bone marrow needs to constantly renew from the stem cell pool. It’s these stem cells that are the most valuable cells in bone marrow transplantation.
The Need for a Bone Marrow Transplant
Some diseases destroy bone marrow leaving patients unable to make new blood cells and therefore vulnerable to infection. Patients may require a bone marrow transplant to survive. These blood cancers include:
- Leukemia
- Lymphoma
- Sickle cell anemia
- Myeloproliferative disorders, and
- Other life-threatening diseases
Some treatments of disease are so severe that they can also destroy a patient’s bone marrow. Big doses of chemotherapy and radiotherapy may be needed to treat advanced cancer and some types of leukaemia after remission.
Types of Bone Marrow Transplants
Bone Marrow Transplants are named based on the relationship between the donor and recipient.
Autologous Bone Marrow Transplant - in some transplants, the donor and recipient are the same person. A patient may have their bone marrow harvested or blood stem cells collected to freeze and store for later use, often after treatment that uses high doses of chemotherapy. When the collected cells are reinfused to the patient, the cells quickly regrow and replace damaged cells. Because the cells are the patient’s own, there are fewer complications than donated bone marrow.
Syngeneic Bone Marrow Transplant - this transplant relates to identical twins. These transplants are usually successful with few complications because the marrow is an exact match however they aren’t suitable for inherited diseases like immune deficiencies.
Allogeneic Bone Marrow Transplant - the most common type of transplant where the donor and recipient are an exact or close bone marrow match. They may be related or not.
Ways to Donate Bone Marrow
There are two ways of supplying bone marrow donations - blood stem cell donation and bone marrow.
Blood Stem Cell Donations - Just like giving blood, stem cell donors are fully awake and provide the donation as blood. Around 90% of all donations are stem cells.

Donated cord (placenta) blood is an increasing source of stem cells being used in transplants instead of bone marrow when a donor can’t be found.
Bone Marrow - The remaining 10% of donations are provided as bone marrow. A doctor uses a syringe to take liquid bone marrow from the back of the pelvic bone which produces blood-forming cells. The donor doesn’t feel any pain as they are asleep under a general anaesthetic.
Around 4-6% of a donor’s bone marrow is needed to save a person’s life. A donor regains their lost bone marrow within six weeks.
How Are Transplant Matches Determined?
Finding a bone marrow donor match is much more difficult than finding a blood donor. Often the only suitable family member matches are siblings, as other relatives aren’t a close enough match to the recipient. But siblings still only have a one in four chance of being a match because we inherit half our tissue type from our mother and half from our father.
The donor and recipient must be a good match in terms of white cell groups. Just as there are multiple blood group types, there are multiple white cell types. There are six Human Leukocyte Antigens or glycoproteins that sit on the surface of most cells in the body. These white cell antigens are designed to initiate an immune response when required.
An extended family member may be a complete match or have five of six HLA antigens needed to be a suitable donor. Doctors expect more complications to occur when the donor and patient match on only five of the antigens, than if they were a full match.

Therefore, most donations are from strangers. Non-related donors are found through worldwide bone marrow registers. Those willing to join the register provide a cell sample through a swab of the inside of their cheek. Doctors aim to have an ethnically diverse range of people on the register to increase the chances of a match being found.
What is the Bone Marrow Transplant Process?
There is a process before and after a bone marrow transplant to ensure the greatest chance of success for the patient.
Pre-Transplant Treatment for the Patient
Once a match is found and doctors decide a bone marrow transplant can proceed, the patient will receive high doses of chemotherapy or total body irradiation. This may be required as:
Conditioning to destroy lymphocytes (so the patient’s body is less likely to recognise the donor marrow is foreign), and to destroy any leukaemia or cancer cells that may cause a relapse in the future.
Not all patients require conditioning. A congenital immune defect won’t recognise foreign donor marrow and a donation from an identical twin is an exact match. The days of conditioning are counted backwards D3, D2, D1 and the day of transplant is D0. The days following transplant are D+1, D+2.
Pre-Transplant Treatment for the Donor
Doctors need to be sure the donor won’t change their mind about the transplant so an interview and medical tests are completed before collection of any cells. The patient’s conditioning treatment means the patient may not survive if the donation doesn’t proceed and no other suitable donors are available.

Stem Cell or Bone Marrow Transplant Day for the Donor
If you are donating stem cells through PBSC, the non-surgical procedure takes three to four hours. For five days prior to donating, the doctor gives you a drug which increases the number of cells in your bloodstream available for transplant.
Like donating plasma, you relax in a chair and some of your blood is removed via a needle in your arm. The blood passes through a machine that removes the blood-forming cells and returns the remaining blood to you via a needle in the other arm. PBSC is a non-surgical procedure.
If you’re required to donate bone marrow rather than blood cells, it’s a surgical procedure that takes around two hours. The doctor uses needles to withdraw liquid marrow from the back of your pelvic bone via two small punctures. If you have the surgery in the morning, you are usually fine to go home in the afternoon. Some people may require overnight observation in the hospital.
Stem Cell or Bone Marrow Transplant Day For the Patient
The donor’s healthy blood-forming cells are infused in the patient’s bloodstream through an intravenous (IV) catheter or tube where they can grow and make healthy red and white blood cells, and platelets.
Following Transplant for the Donor
The site of the syringe injections may be sore for a few days after donation, but paracetamol is usually the only treatment required.
A donor will make enough stem cells or bone marrow within six weeks to replace those lost through donation. There are no lasting side effects for the vast majority of donors. You can return to normal routine and activities within a couple of days.
Following Transplant For the Patient
It takes two to four weeks before marrow cells divide and patients’ blood count improves. Infection often occurs from germs on the patient’s skin, nose and gut entering the bloodstream. They may need antibiotics to fight the infection.
Like any transplant, rejection of the donor tissue is a possibility. If the donor’s lymphocytes realise the recipient’s cells are different, they may reject the tissues of the recipient. The tissues most likely affected are the skin, gut, and liver and can cause rashes, diarrhoea, and jaundice.
Patients may have ongoing problems digesting food and poor liver function requiring changes in diet.
Are There any Risks for Donors?
All medical procedures carry a certain amount of risk, but the risks to a bone marrow donor is minimal. The Mayo Clinic reported the most serious side effect to consider is the use of anaesthetic during the procedure.
Side Effects of a Bone Marrow Donation
Donors may experience one or more of the following side effects of donating bone marrow:
- Dehydration
- Dizziness
- Fatigue
- Bruising and discomfort
- Infection
- Citrate reaction
- Arterial puncture
Who Can Donate Bone Marrow?
Most people assume any willing adult can donate bone marrow, but that’s not the case, only a minority of the population are suitable.

Age
The ideal bone marrow donors sought to register are between the ages of 18 and 35 years of age.
Most doctors seek donors aged 18-35 years because young donors provide the best outcome for sick recipients. The transplant is more likely to be a success with fewer complications using a young adult’s cells.
Gender
Doctors prefer male donors because they are on average larger than females and can donate more bone marrow. Men also don’t get pregnant or breastfeed which prevents females from donating during this stage of life.
Medical History
Before registering as a donor, they conduct brief medical checks to ensure you are suitable. If you’re asked to donate, they conduct a thorough physical examination and tests first.
You may not be considered a suitable bone marrow donor if you have:
- HIV (AIDS)
- Severe arthritis
- Asthma requiring daily/regular medications
- Autoimmune disease that impacts your whole body (more than one organ)
- Elevated blood pressure
- Bleeding problems
- A brain injury or have had brain surgery
- Cancer that required chemotherapy
- Serious mental health problems
- Chronic neck, back, spine pain
- Chronic kidney or liver disease such as Hepatitis B or C
- Underweight or overweight BMI that could threaten your safety
- Life threatening allergies to latex or medications
FAQ’s About Bone Marrow Donations
Some of the most common questions about bone marrow donations include:
Can a Minor Donate Bone Marrow?
Worldwide, there have been questions around whether a child should donate bone marrow to their sick sibling. Desperate parents have had another child via IVF to provide the stem cells their sick child needs. Both scenarios raise questions around ethics.
The parents may need to go to court to gain approval because they can’t sign a release or give consent on their child’s behalf to donate. In most cases, the court or ethics committee has granted approval because there is a family and emotional tie between donor and recipient.
Who Pays for a Transplant?
In Australia, Medicare pays the costs associated with joining the register and for donating blood and bone marrow.
Can I Decide Whether to Donate Stem Cells or Bone Marrow?
The patient’s doctor will decide which is the best form of donation.
What Happens if I Change My Mind?
If you join the Bone Marrow Register, you should be willing to donate anonymously to anyone in Australia or overseas if you’re found to be a match. You don’t need to travel overseas for the donation. Being on the donor register doesn’t commit you to go ahead with the procedure, it’s a voluntary procedure. But you should think twice before joining the register.
Why Does Ethnicity Matter When Finding a Bone Marrow Match?
Ethnic background impacts on the human leukocyte antigen (HLA) type, so the best chance of finding a donor is with someone of the same ethnic background. It’s important that the donor registry contains a wide range of ethnic backgrounds to increase the chance that patients can be matched.
If you’re interested in finding out more about joining the bone marrow donor register, visit the Australian Bone Marrow Donor Registry or call the Red Cross Blood Service on 13 14 95 to book an appointment.